Epitope spreading is a phenomenon where the immune response expands beyond the original targeted epitopes to recognize additional epitopes on the same or different antigens. This process often occurs during chronic infections, prolonged inflammation, or autoimmune disease progression, leading to a broader and sometimes harmful immune reaction. It plays a key role in the development and persistence of autoimmune conditions.
Understanding epitope spreading is key to appreciating immune response dynamics and their pathological role. It enhances responses against pathogens/tumors but can also drive chronic, diverse autoimmune disease. This article explores its mechanisms, types, implications in autoimmunity/tumor immunity, and the role of epitope mapping.
Mechanisms Driving Epitope Spreading
Epitope spreading is far from a random event; it is a meticulously orchestrated process involving a cascade of cellular and molecular occurrences. At its core lies the sophisticated interplay of antigen processing, presentation, and lymphocyte activation.
Initial Trigger and Antigen Release
The process often begins when tissue damage occurs. Whether induced by infection, inflammation, or the destruction of self-tissue, this damage leads to the release of intracellular antigens. These released antigens encompass both the molecules that triggered the initial immune response and previously sequestered self-antigens.
Antigen Processing and Presentation
Following release, these antigens are taken up by Antigen-Presenting Cells (APCs), particularly dendritic cells (DCs), which are highly effective at initiating immune responses. Within APCs, ingested proteins are degraded into smaller peptide fragments. These fragments then bind to Major Histocompatibility Complex (MHC) molecules. The resulting peptide-MHC complexes are subsequently displayed on the surface of the APCs, making them available for recognition by T cells.
Expansion of the Immune Response
- Activation by Primary Epitopes: The initial immune response is typically initiated by T cells recognizing and binding to the primary epitopes presented by APCs.
- Exposure and Presentation of New Epitopes: A persistent inflammatory environment plays a crucial role by acting as a potent stimulus. This sustained inflammation promotes the continuous uptake and processing of antigens by APCs. During this ongoing process, APCs are likely to process and present additional epitopes from the antigen molecule. These include epitopes that were not readily accessible or presented under normal physiological conditions, often referred to as cryptic epitopes.
- Recruitment of Naive or Low-Affinity Lymphocytes: The presentation of these new epitopes by APCs can then activate naive T cells or reactivate T cells with low affinity for the primary epitopes but higher affinity for the newly presented ones.
- T Cell and B Cell Collaboration: Activated T cells, especially CD4+ helper T cells, recognizing primary epitopes, secrete cytokines that enhance the inflammatory response and provide essential help for B cell activation. Activated B cells function as efficient APCs themselves. They can capture antigens via their B cell receptor (which recognizes specific epitopes), internalize and process them, and present peptide fragments via MHC-II molecules to T cells. T cells recognizing these peptides can then help the B cells produce antibodies against the newly recognized epitopes.
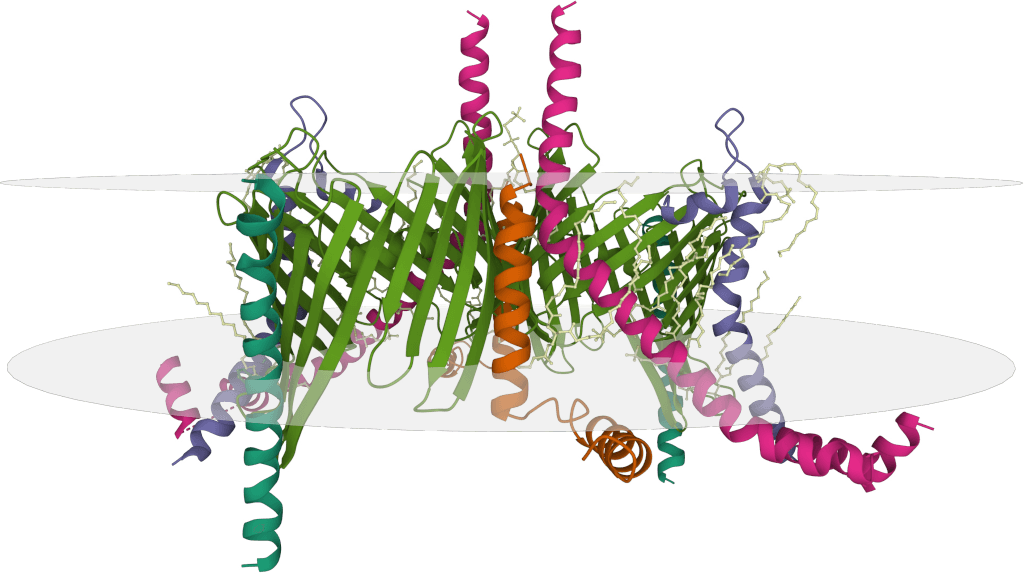
 Figure 1. Intramolecular B Cell Epitope Spreading Mechanism. (A) Activation through T cell intrastructural help. (B) Clustering of BCRs on a specific epitope of the antigen (Ag). B cells endocytose the antigen, process it, and present new epitopes via MHC II to T cells, leading to reciprocal activation of B cells and production of antibodies targeting the newly presented epitope. (Cornaby C, et al., 2015)
Figure 1. Intramolecular B Cell Epitope Spreading Mechanism. (A) Activation through T cell intrastructural help. (B) Clustering of BCRs on a specific epitope of the antigen (Ag). B cells endocytose the antigen, process it, and present new epitopes via MHC II to T cells, leading to reciprocal activation of B cells and production of antibodies targeting the newly presented epitope. (Cornaby C, et al., 2015)
The Cascade Effect and Influencing Factors
This sequence of events results in a gradual shift in the immune response's target from the initial epitopes to other epitopes on the same molecule or on different molecules. This creates a sequential determinant spreading cascade. This progression is influenced by various factors, including the intensity and duration of inflammation, the specific type and functional state of the APCs involved, and the overall diversity of the individual's immune cell repertoire.
Types of Epitope Spreading
Epitope spreading can be broadly categorized into two main types based on the relationship between the newly recognized epitopes and the antigen carrying the initial epitope:
Intramolecular Epitope Spreading
This refers to the situation where the immune response expands from one region of an antigen molecule to target other epitopes located within the same antigen molecule. For instance, an immune response initially directed against the N-terminus of a protein might subsequently broaden to include epitopes on the C-terminus or in the central regions of that same protein.
Intermolecular Epitope Spreading
This type of spreading occurs when the immune response expands from an epitope on one antigen molecule to target epitopes located on a different antigen molecule. These distinct antigen molecules are typically found within the same tissue or cellular complex. For example, during tissue destruction, cell lysis releases a variety of proteins. An immune response initially targeting an epitope on one of these proteins might later expand to include epitopes on other proteins present in the same damaged cells or tissue structures.
Both intramolecular and intermolecular epitope spreading can occur concurrently, collectively driving the diversification of the immune response targets.
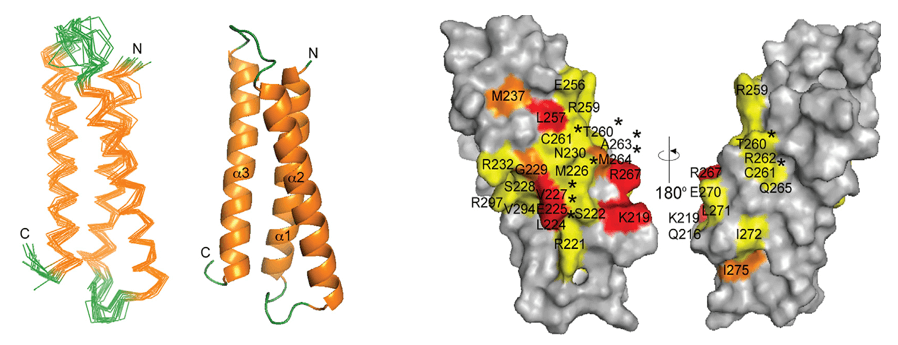
 Figure 2. Illustration of T-cell epitope spreading. The immune response begins with dominant initiating T-cell epitopes and may expand to additional epitopes within the same antigen (intramolecular spreading) or to epitopes from different antigens (intermolecular spreading), contributing to a broader autoimmune response. (Kellermann G, et al., 2024)
Figure 2. Illustration of T-cell epitope spreading. The immune response begins with dominant initiating T-cell epitopes and may expand to additional epitopes within the same antigen (intramolecular spreading) or to epitopes from different antigens (intermolecular spreading), contributing to a broader autoimmune response. (Kellermann G, et al., 2024)
Epitope Spreading in Autoimmune Diseases
Epitope spreading is a central concept for understanding the initiation and progression of autoimmune diseases. In these conditions, the immune system mistakenly attacks the body's own tissues and cells. The initial autoimmune reaction may target only a limited number of epitopes on self-antigens. This initial trigger can be multifactorial, potentially initiated by infections, tissue damage, or other factors, such as:
- Bystander Activation: In the presence of infection or tissue damage, the local inflammatory environment can non-specifically activate self-reactive lymphocytes that happen to be present.
- Molecular Mimicry: This occurs when epitopes on a pathogen share structural similarity with epitopes on self-antigens, leading to an immune response directed against the pathogen mistakenly attacking self-tissue. While distinct in mechanism from epitope spreading, molecular mimicry can potentially initiate the initial self-reactive response, which is then amplified and broadened through epitope spreading.
Once the initial autoimmune reaction takes hold and leads to tissue damage, the damaged cells release an increased array of self-antigens. Other epitopes within these newly exposed or released self-antigens can then be captured and presented by APCs, triggering an immune response against these novel epitopes, thus leading to epitope spreading. This spreading causes the autoimmune reaction to propagate beyond the initial targets, attacking other components within the same tissue or even other tissues throughout the body that express related antigens.
Epitope Spreading in Multiple Sclerosis (MS)
In MS, the immune system attacks the myelin sheath in the central nervous system. The initial immune response might target specific epitopes on myelin basic protein (MBP) or proteolipid protein (PLP). As the disease progresses and myelin is destroyed, increasing amounts of myelin components are released. The immune response then expands to include epitopes on MBP, PLP, and other myelin proteins like myelin oligodendrocyte glycoprotein (MOG). Both intramolecular and intermolecular epitope spreading are considered significant contributors to the chronicity and relapsing-remitting cycles characteristic of MS.
Epitope Spreading in Systemic Lupus Erythematosus (SLE)
SLE is a systemic autoimmune disease affecting multiple organ systems, characterized by the production of autoantibodies against various nuclear components. Studies indicate that the targets of autoantibodies in SLE patients diversify as the disease progresses, expanding from initial epitopes on a few nuclear antigens to epitopes on other nuclear antigens and even cytoplasmic antigens. This phenomenon is believed to contribute significantly to the diverse clinical manifestations and chronic nature of SLE.
The significance of epitope spreading in autoimmune diseases lies in its ability to explain why these conditions often worsen over time, with the scope of attack broadening, and why therapies targeting only a single self-antigen are often insufficient to achieve a complete cure.
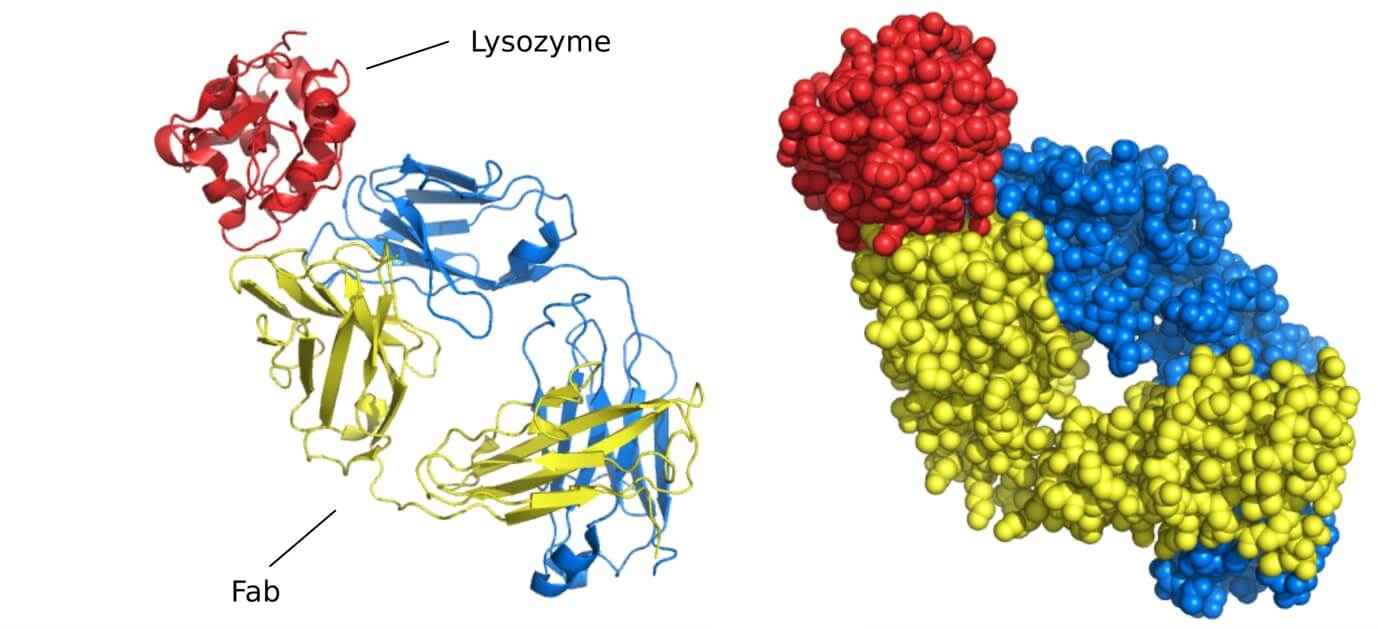
 Figure 3. Epitope Spreading in Lupus Nephritis. Early nucleosome–autoantibody complex formation in the mesangium causes mild kidney damage. As the disease progresses, epitope spreading triggers production of autoantibodies targeting histones and glomerular autoantigens, resulting in immune complex deposition and worsening kidney damage. Kidney tertiary lymphoid structures (TLSs) further contribute to localized immune responses, disease progression, and poor treatment outcomes. (Strizzi C T, et al., 2024)
Figure 3. Epitope Spreading in Lupus Nephritis. Early nucleosome–autoantibody complex formation in the mesangium causes mild kidney damage. As the disease progresses, epitope spreading triggers production of autoantibodies targeting histones and glomerular autoantigens, resulting in immune complex deposition and worsening kidney damage. Kidney tertiary lymphoid structures (TLSs) further contribute to localized immune responses, disease progression, and poor treatment outcomes. (Strizzi C T, et al., 2024)
Epitope Spreading in Cancer Immunotherapy
In the context of tumor immunity, epitope spreading is generally considered a favorable phenomenon that helps to amplify the anti-tumor immune response. Tumor cells express numerous aberrant proteins known as Tumor-Associated Antigens (TAAs) or Tumor-Specific Antigens (TSAs). The initial anti-tumor immune response might primarily focus on one or two highly immunogenic tumor epitopes.
However, following therapeutic interventions such as chemotherapy, radiotherapy, targeted therapy, or certain immunotherapies that induce tumor cell lysis and death, a substantial quantity of tumor antigens is released into the tumor microenvironment. These antigens are subsequently captured, processed, and presented by APCs. The immune response can then broaden to include other epitopes on these newly exposed tumor antigens.
Benefits of Tumor Epitope Spreading
The broadening of the immune response to include other epitopes on these newly exposed tumor antigens offers several crucial benefits:
Overcoming Tumor Heterogeneity
Tumors often exhibit high internal antigenic heterogeneity. Through epitope spreading, the immune system gains the ability to recognize and attack tumor cells expressing a wider array of antigens, including those that lack the specific antigen targeted by the initial response. This leads to a more comprehensive elimination of the tumor cell population.
Preventing Immune Escape
Tumor cells can evade immune recognition by downregulating or losing the expression of a specific target antigen. Epitope spreading ensures that the immune system simultaneously recognizes multiple tumor epitopes, making it significantly less likely for tumor cells to escape detection simply by losing a single antigen.
Enhancing Immunotherapy Efficacy
Epitope spreading can significantly enhance the effectiveness of various immunotherapy strategies, such as tumor vaccines, oncolytic virus therapies, and CAR T cell therapy. By inducing tumor cell death and antigen release, these therapies can trigger further epitope spreading, thereby amplifying and diversifying the anti-tumor immune response and improving overall therapeutic outcomes. Effective CAR T treatment, for instance, has been shown to induce host immune responses against non-targeted antigens, representing beneficial epitope spreading that enhances anti-tumor effects.
Therefore, in tumor immunology, inducing or enhancing epitope spreading is recognized as a vital strategy for improving the efficacy of immunotherapy, broadening the scope of the anti-tumor response, and ultimately helping to prevent tumor recurrence and metastasis.
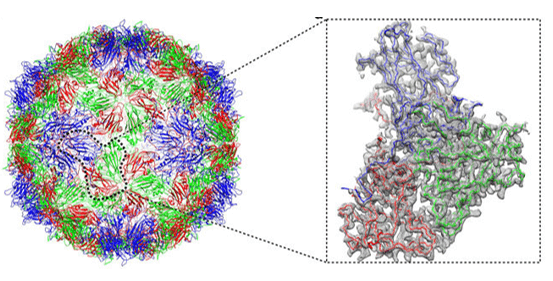
 Figure 4. Illustration of the antigen spread process after immunotherapy. (A) Tumor cell death releases additional antigens. (B) Dendritic cells process and present these antigens to T-cells. (C) T-cells are primed against a broader set of tumor antigens. (D) This expands the diversity and concentration of tumor-specific T-cells. (E) The activated T-cells enhance antitumor immune responses beyond the initially targeted antigen. (Gulley J L, et al., 2017)
Figure 4. Illustration of the antigen spread process after immunotherapy. (A) Tumor cell death releases additional antigens. (B) Dendritic cells process and present these antigens to T-cells. (C) T-cells are primed against a broader set of tumor antigens. (D) This expands the diversity and concentration of tumor-specific T-cells. (E) The activated T-cells enhance antitumor immune responses beyond the initially targeted antigen. (Gulley J L, et al., 2017)
Epitope Spreading vs Molecular Mimicry
While both epitope spreading and molecular mimicry can contribute to autoimmunity, their underlying mechanisms differ.
- Molecular Mimicry: This refers to the structural similarity between peptide sequences from a pathogen and those from a self-antigen. This similarity can lead to an immune response initially directed against the pathogen mistakenly attacking self-antigens. Molecular mimicry is often considered a potential trigger in the induction phase of initial autoimmune responses.
- Epitope Spreading: This phenomenon describes the broadening of immune targets from the initial inciting epitopes to other epitopes on the same or different antigens, occurring on the basis of an already established immune response. It is primarily considered a mechanism driving the progression and maintenance of autoimmune diseases.
In essence, molecular mimicry can be seen as a "trigger" for the initial self-reactive response, while epitope spreading acts as a "spreading mechanism" that expands and perpetuates the autoimmune attack. It is worth noting that in some scenarios, an initial self-reactive response triggered by molecular mimicry might subsequently induce epitope spreading.
 Figure 5. Molecular Mimicry and Epitope Spreading in Autoimmunity. Diagram illustrating how molecular mimicry between viral antigens (e.g., EBNA-1) and self-antigens can trigger autoimmunity. Cross-reactive antibodies form immune complexes that are processed by APCs, activating autoreactive T cells due to defective tolerance. These T cells assist autoreactive B cells, promoting a broader autoimmune response through epitope spreading, where B cells internalize and present peptides from self-proteins sharing epitopes with viral antigens. (Jog N R, et al., 2021)
Figure 5. Molecular Mimicry and Epitope Spreading in Autoimmunity. Diagram illustrating how molecular mimicry between viral antigens (e.g., EBNA-1) and self-antigens can trigger autoimmunity. Cross-reactive antibodies form immune complexes that are processed by APCs, activating autoreactive T cells due to defective tolerance. These T cells assist autoreactive B cells, promoting a broader autoimmune response through epitope spreading, where B cells internalize and present peptides from self-proteins sharing epitopes with viral antigens. (Jog N R, et al., 2021)
The Role of Epitope Mapping in Understanding Epitope Spreading
To fully understand the dynamic process of epitope spreading and its implications in disease, it is essential to accurately identify and quantify the specific antigen epitopes recognized by the immune system at different stages.
Epitope mapping is a technique used to determine which specific regions on an antigen molecule are recognized and bound by antibodies or T cells. By performing epitope mapping on serum samples (for B cell epitopes) or lymphocytes (for T cell epitopes) collected from patients at various disease stages, researchers can gain critical insights:
- Identify the Initial Epitopes: Determine the primary antigen epitopes that are predominantly recognized during the early stages of the disease or immune response initiation.
- Track the Progression of Epitope Spreading: Compare epitope profiles at different time points to observe how the immune response targets broaden from the initial epitopes to include novel ones.
- Distinguish Intramolecular and Intermolecular Spreading: Ascertain whether the newly recognized epitopes are located on the same antigen or on different antigens.
- Identify Potentially Pathogenic Epitopes: Pinpoint epitopes whose recognition correlates with disease activity or severity.
- Discover Novel Autoantigens or Tumor Antigens: Through systematic epitope analysis, it is possible to identify previously unknown antigens or their epitopes that are recognized by the immune system.
A variety of epitope mapping techniques are available to study epitope spreading, including mass spectrometry-based approaches, array-based methods, phage display technology, and screening using synthetic peptide libraries. The choice of the appropriate technique depends on the research objectives, sample type, and the nature of the antigen.
Select Service
By providing a detailed map of the immune targets, epitope mapping allows researchers to dissect the complex evolution of the immune response during epitope spreading, offering invaluable data for both basic research and clinical applications.
At Creative Biostructure, we provide expert epitope mapping services to support your immunology research. Our team offers a full range of solutions to accurately identify immune targets across disease stages. Whether your work focuses on autoimmune disorders, cancer immunotherapy, or therapeutic antibody development, we are here to help. Contact us to learn how our customized epitope mapping services can accelerate your discoveries.
References
- Tuohy V K, Yu M, Yin L, et al. The epitope spreading cascade during progression of experimental autoimmune encephalomyelitis and multiple sclerosis. Immunological reviews. 1998, 164(1): 93-100. https://doi.org/10.1111/j.1600-065X.1998.tb01211.x
- Hardwick N, Chain B. Epitope spreading contributes to effective immunotherapy in metastatic melanoma patients. Immunotherapy. 2011, 3(6): 731-733. https://doi.org/10.2217/imt.11.62
- Cornaby C, Gibbons L, Mayhew V, et al. B cell epitope spreading: mechanisms and contribution to autoimmune diseases. Immunology letters. 2015, 163(1): 56-68. https://doi.org/10.1016/j.imlet.2014.11.001
- Gulley J L, Madan R A, Pachynski R, et al. Role of antigen spread and distinctive characteristics of immunotherapy in cancer treatment. JNCI: Journal of the National Cancer Institute, 2017, 109(4): djw261. https://doi.org/10.1093/jnci/djw261
- Didona D, Di Zenzo G. Humoral epitope spreading in autoimmune bullous diseases. Frontiers in immunology. 2018, 9: 779. https://doi.org/10.3389/fimmu.2018.00779
- Conde E, Vercher E, Soria-Castellano M, et al. Epitope spreading driven by the joint action of CART cells and pharmacological STING stimulation counteracts tumor escape via antigen-loss variants. Journal for Immunotherapy of Cancer. 2021, 9(11): e003351. https://doi.org/10.1136/jitc-2021-003351
- Jog N R, James J A. Epstein Barr virus and autoimmune responses in systemic lupus erythematosus. Frontiers in immunology, 2021, 11: 623944. https://doi.org/10.3389/fimmu.2020.623944
- Strizzi C T, Ambrogio M, Zanoni F, et al. Epitope Spreading in Immune-Mediated Glomerulonephritis: The Expanding Target. International Journal of Molecular Sciences. 2024, 25(20): 11096. https://doi.org/10.3390/ijms252011096
- Suliman B A. Potential clinical implications of molecular mimicry‐induced autoimmunity. Immunity. Inflammation and Disease. 2024, 12(2): e1178. https://doi.org/10.1002/iid3.1178
- Kellermann G, Leulliot N, Cherfils-Vicini J, et al. Activated B-Cells enhance epitope spreading to support successful cancer immunotherapy. Frontiers in Immunology. 2024, 15: 1382236. https://doi.org/10.3389/fimmu.2024.1382236