Exosome Wound Healing and Bone Regeneration Studies
Regenerative medicine faces a dual challenge: promoting rapid wound closure while preventing fibrosis (scarring), and accelerating bone union in complex fractures. MSC Exosomes have emerged as potent mediators of this process, orchestrating the complex interplay between blood vessel formation and tissue remodeling.
We provide specialized Exosome Wound Healing and Bone Regeneration solutions. Whether you are developing a topical formulation for diabetic ulcers or an engineered scaffold for bone defects, our platform offers the functional bioassays and in vivo models needed to validate the regenerative potency of your exosome product.
The Mechanism of Exosome-Mediated Regeneration
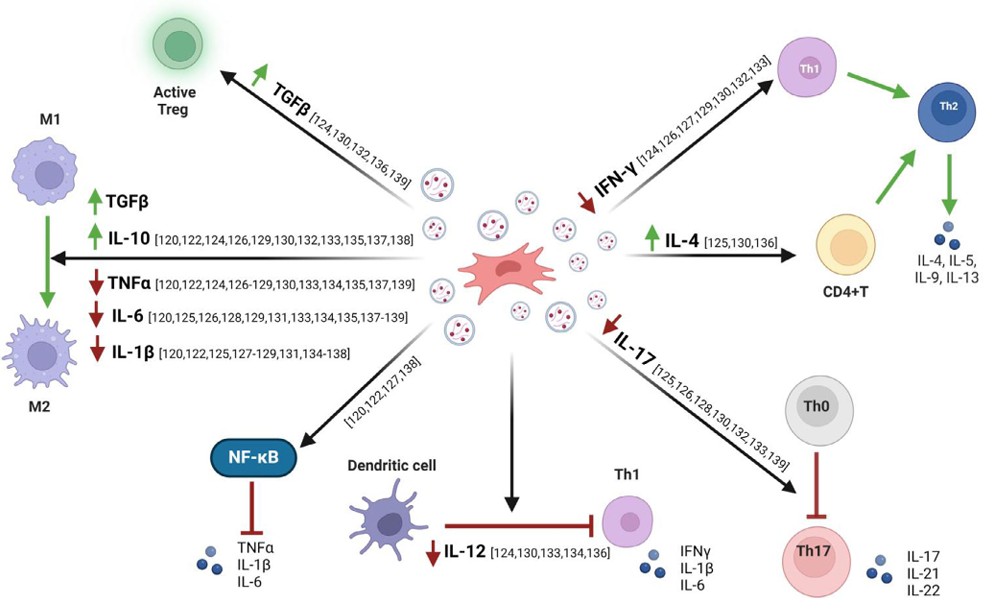
Exosomes promote healing not by one single pathway, but by activating a regenerative network.
- Promoting Angiogenesis: Both bone and skin repair rely on blood supply. Exosomes deliver pro-angiogenic factors (e.g., VEGF, miRNA-126) to endothelial cells, stimulating the formation of new blood vessels.
- Collagen Remodeling: In wound healing, exosomes regulate fibroblast activity to ensure orderly collagen deposition, accelerating closure while minimizing hypertrophic scarring.
- Osteogenesis Induction: For bone repair, exosomes stimulate the proliferation and differentiation of osteoblasts while inhibiting osteoclasts, accelerating mineralization and fracture union.
- Diabetic Complications: Chronic wounds often fail to heal due to ischemia. Exosomes can rescue cells from high-glucose induced apoptosis and restore the regenerative microenvironment.
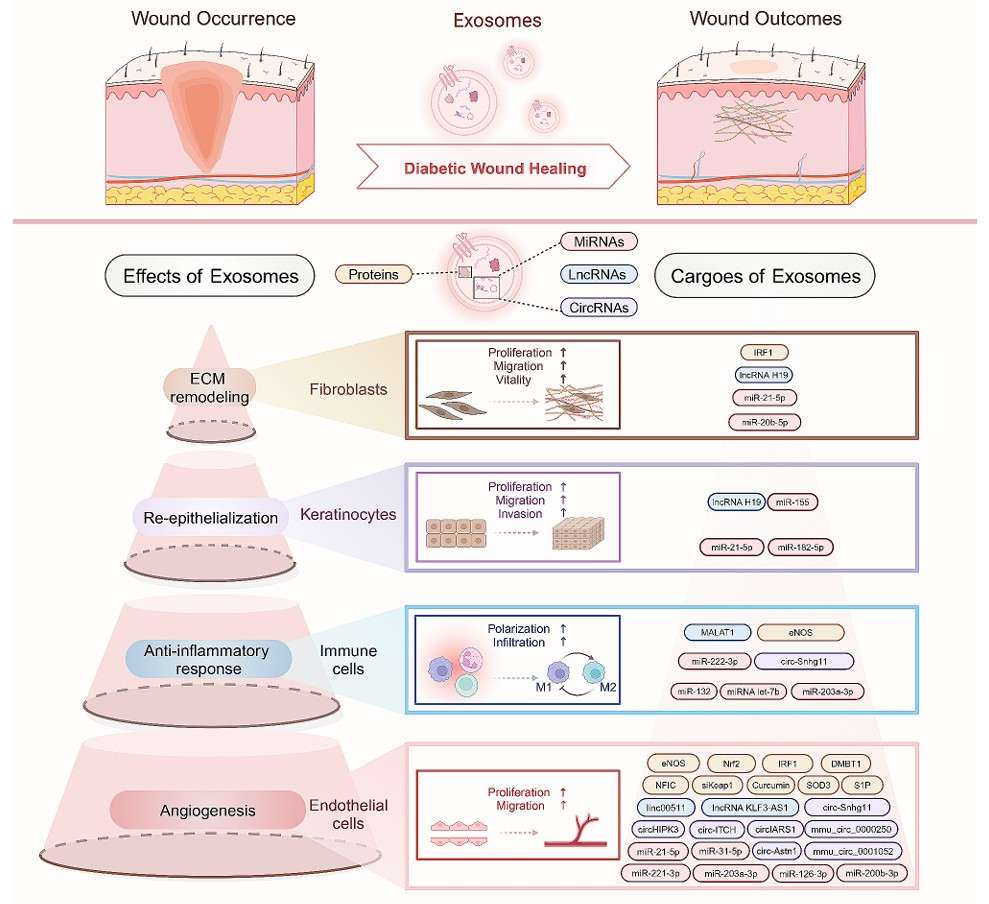 Figure 1. Exosomes carrying ncRNAs and proteins enhance diabetic wound healing by modulating cell behavior and functions. (Li Y, et al., 2024)
Figure 1. Exosomes carrying ncRNAs and proteins enhance diabetic wound healing by modulating cell behavior and functions. (Li Y, et al., 2024)
Our Regeneration Research Workflow
We offer a pipeline optimized to test bioactivity in relevant skin and bone models.
| Development Phase | Our Specialized Approach & Solution | Key Services Applied |
|---|---|---|
| Bioactive Cargo Profiling | Growth Factor Analysis: We profile the exosome cargo to quantify key regenerative factors. This includes ELISA for VEGF/bFGF and sequencing for miRNAs known to regulate the Wnt/β-catenin or TGF-β pathways. | Exosome Proteomics, Exosomal Small RNA and miRNA Sequencing |
| In Vitro Angiogenesis | Vascularization Assays: Since blood supply is critical, we use HUVEC Tube Formation and aortic ring assays as a primary potency release test to verify that your exosomes can stimulate vessel growth. | Angiogenesis and Stem Cell Functional Assays |
| Tissue-Specific Assays | Skin vs. Bone: For skin, we perform Scratch Migration assays on fibroblasts. For bone, we conduct Alizarin Red staining on MSCs to quantify calcium deposition (mineralization) induced by your exosomes. | In Vitro Exosome Functional Assays |
| In Vivo Efficacy | Defect Models: We utilize established animal models, such as the Full-Thickness Skin Excision model (for wounds) or the Calvarial Defect model (for bone), to prove accelerated healing rates compared to controls. | In Vivo Exosome Functional Assays |
Core Technologies for Tissue Engineering
We deploy specific functional assays to quantify regeneration.
Angiogenesis Potency Testing
The Driver of Repair: Rapid vascularization is the rate-limiting step in tissue repair. We utilize a standardized HUVEC Tube Formation assay, analyzing total tube length, branching points, and loop numbers. This provides a quantitative metric of your exosome's angiogenic potency, which correlates strongly with in vivo success.
Osteogenic Differentiation Assays
Validating Bone Growth: To prove osteoinductive potential, we treat stem cells with your exosomes and measure the expression of bone markers (ALP, Runx2, OCN). We confirm functional mineralization using Alizarin Red S staining, providing visual and quantitative proof that your product drives bone formation.
Fibrosis & Scarring Analysis
Quality of Healing: Speed isn't everything; quality matters. We analyze the ratio of Collagen I vs. Collagen III and the expression of alpha-SMA (a marker of myofibroblasts) to determine if your exosome treatment promotes scar-free healing or merely rapid fibrosis.
Application Spotlight: Exosomes Accelerate Fracture Healing
This analysis highlights the dual mechanism of exosomes in bone repair: promoting both blood vessel formation and bone cell differentiation to treat nonunion fractures.
Featured Technologies:
- MSC Exosome Isolation
- Angiogenesis & Osteogenesis Assays
Literature Interpretation:
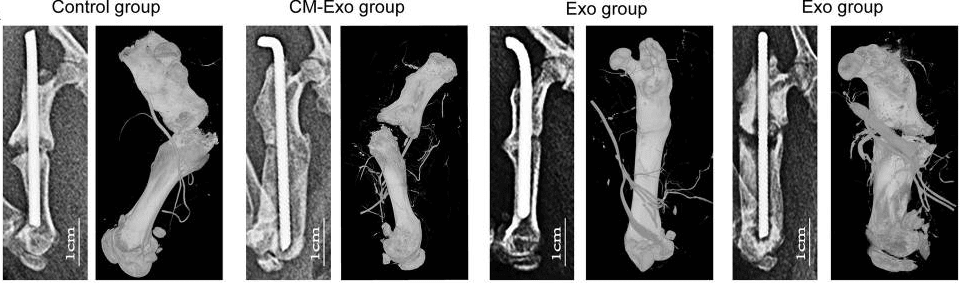 Figure 2. Micro-CT imaging of vasculature at the fracture site on postoperative week 20, showing increased vascular branches in the Exo group. (Zhang L, et al., 2020)
Figure 2. Micro-CT imaging of vasculature at the fracture site on postoperative week 20, showing increased vascular branches in the Exo group. (Zhang L, et al., 2020)
Fracture nonunion (failure to heal) is a major clinical complication often caused by poor blood supply and insufficient bone formation. Researchers investigated whether exosomes derived from Bone Marrow MSCs (BMSCs) could rescue this condition. They injected these exosomes into a rat model of fracture nonunion. The BMSC-exosome treatment significantly accelerated fracture healing compared to the control group. Histological analysis revealed a dual effect: the exosomes enhanced angiogenesis (increasing vessel volume) and simultaneously promoted osteogenesis (increasing bone volume and mineral density). This study provides compelling evidence that MSC exosomes can orchestrate the complex microenvironment required for bone repair, validating their potential as a cell-free therapy for orthopedic injuries.
Start Your Regeneration Project
We make getting started straightforward. Our process is designed to be collaborative and transparent.
How It Works: Our Project Pathway
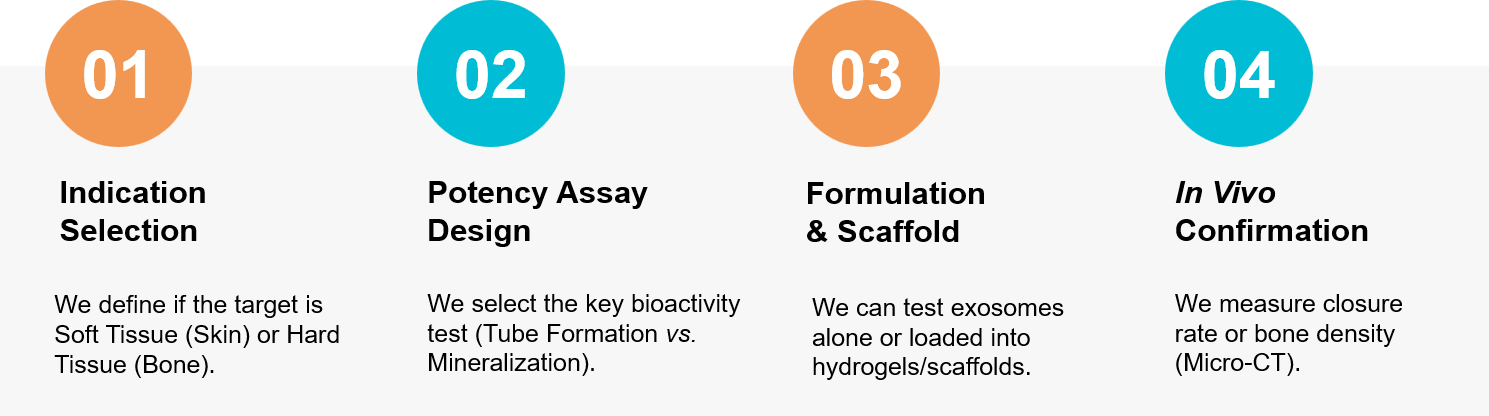 Figure 3. Our workflow for validating the dual regenerative potential of exosomes in vascularization and tissue remodeling. (Creative Biostructure)
Figure 3. Our workflow for validating the dual regenerative potential of exosomes in vascularization and tissue remodeling. (Creative Biostructure)
Ready to validate the regenerative power of your exosomes? Our scientific team is available for a free consultation to discuss your wound healing or bone repair strategy. Contact us today to discuss your project.
References
- Li Y, Zhu Z, Li S, et al. Exosomes: compositions, biogenesis, and mechanisms in diabetic wound healing. J Nanobiotechnology. 2024 Jul 5;22(1):398.
- Zhang L, Jiao G, Ren S, et al. Exosomes from bone marrow mesenchymal stem cells enhance fracture healing through the promotion of osteogenesis and angiogenesis in a rat model of nonunion. Stem Cell Res Ther. 2020 Jan 28;11(1):38.